In the no-longer-available 2021 HIV Surveillance Report (archived), the CDC found that across seven major U.S. cities, more than 2 in 5 trans women tested positive for HIV. Among Black trans women, the rate soars to 62%, compared to 35% of Hispanic/Latina and 17% of white trans women—figures that lay bare a public health crisis shaped by racism and transmisogyny, and the systemic neglect at their intersection.
Despite the life-saving potential of pre-exposure prophylaxis (PrEP) medication, both uptake and adherence remain uneven across populations that face disparate systemic violence and barriers to care. “There are systemic historical barriers that remain in place, “ says Dr. Sean Arayasirikul, a medical sociologist and associate professor at UC Irvine who has worked to address these disparities both in direct public health service and as a researcher. “Trusting the medical system, trusting pharmaceutical and biomedical intervention is a major hurdle,” they tell me, and also just the beginning.
For experts and community leaders like Arayasirikul, these systemic barriers are clear: a lack of culturally competent care, exclusion from more than a decade of mainstream messaging, and a history of being overlooked or non-consensually experimented on by both researchers and direct service providers. Today we explore the roots of those disparities, and what it will take to build trust and equitable, effective access to HIV prevention, especially for Black trans women.
A Crisis in Action, Access, and Awareness
Since the introduction of PrEP more than a decade ago, public health campaigns and clinical outreach efforts have overwhelmingly centered cisgender men who have sex with men (MSM). Transgender women have largely been expected to proactively seek out PrEP on their own, navigating systems that do not center their needs or experiences. A 2020 study in the Journal of the International AIDS Society found that trans women were more likely than MSM to live below the poverty limit, to be unemployed or unhoused. They were also less likely than MSM to have heard of PrEP or had a conversation with a healthcare provider about it. As a result of these barriers, critical gaps in access, adherence, and engagement persist.
“Because of the very targeted marketing that pharmaceutical companies have done,” Dr. Arayasirikul says, “from the early rollout of PrEP focused on cis men who have sex with men, and so with that backdrop there has been a misconception which serves as a barrier for trans women to acknowledge that PrEP might be a viable option for HIV prevention for them.”
This concern was echoed by Joelle Espeut, the Program and Advocacy Director at The Normal Anomaly Initiative, which seeks to center care for Black and Brown women in Houston, Texas, with a particular focus on HIV testing and prevention for queer and trans Black women. “Many black women don’t even really know that PrEP is for them,” Espeut tells me, a problem exacerbated by a lack of healthcare spaces centering their needs. “One of the things that we’ve seen is Black and Brown women don’t engage in sexual health direct services…there isn’t any programming tailored to them, and there aren’t any spaces for Black and Brown women to come together to openly talk about their sexual health. No one had ever created something that centered them in the conversation about PrEP.”
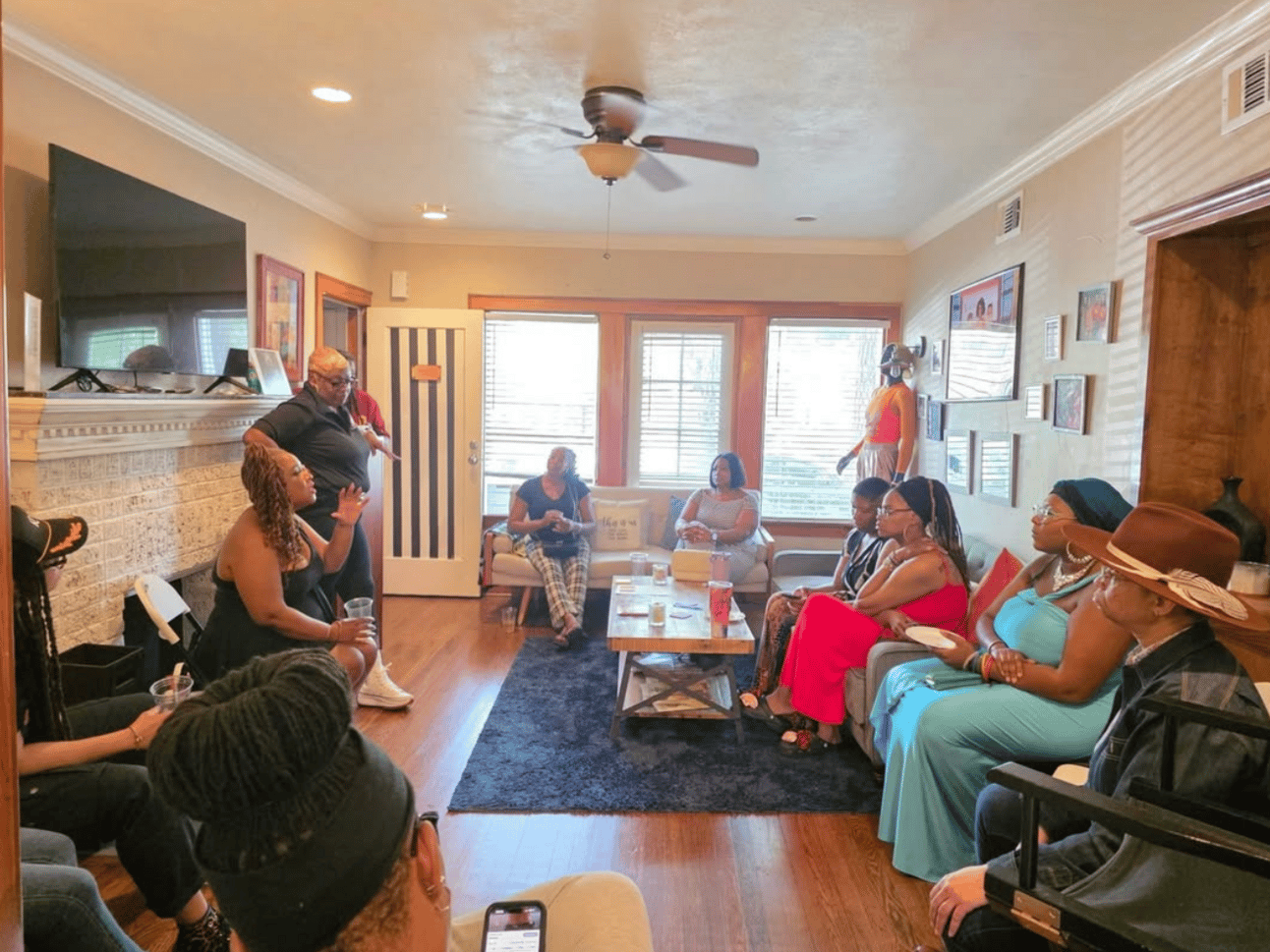
Gathering at The Normal Anomaly Initiative
That is, Arayasirikul says, just the beginning of how inequities in HIV vulnerability and acquisition show up. “Racial and ethnic disparities and inequities [in PrEP use] mirror the same root causes of disproportionate HIV burden among communities and populations of trans women of color, who don’t have access to gender-affirming care, to secure and stable employment.”
National PrEP dispensing grew by 12.5% quarterly between 2016 and 2018, and continued to rise more modestly thereafter. But according to the recent data, transgender women remain markedly underrepresented in both prescription and adherence rates. Trans women of color face overlapping structural disadvantages that directly shape their HIV vulnerability. The SHINE Study published in the American Journal of Public Health in 2015 found that Black and Latina trans women reported significantly lower educational attainment and higher levels of housing instability compared to their white peers. Many had been forced out of their homes at a young age and into unstable living situations where sex work often became their only available means of economic survival.
These patterns continue into adulthood. A 2024 study to which Dr. Arayasirikul contributed revealed that adult trans women with cisgender male partners—who are often navigating societal and interpersonal dynamics shaped by gendered power and economic dependency—reported substantially higher rates of condomless receptive anal sex, participation in sex work, and likely as a result of their survival sex work, higher rates of incarceration, which in turn leads to greater stress, stigma, and systemic oppression, continuing a cycle of increased vulnerability.
Diversity of Tactics
Despite years of exclusion from mainstream public health messaging, Black trans women have long been at the forefront of community-based solutions. Peer-led interventions have proven to be not just effective, but essential. Black trans women often serve as informal PrEP advocates—trusted, visible figures encouraging others to consider and sustain HIV prevention strategies. This kind of leadership challenges the medical establishment’s top-down approach and re-centers those most affected as the drivers of change.
Experts recommend a variety of different, simultaneous approaches to improve access, uptake, and adherence to PrEP protocols:
Peer-led interventions
“What we found was that what was really helpful, that really kind of shifted our thinking, was to develop a standalone prep only clinic…where we had trans folks working intake as well as navigation and counseling around prep,” Dr. Arayasirikul explains. Having community members in leadership and front-line roles created immediate buy-in for members of the targeted community.
This is going to mean that researchers and care providers need to extend some faith to the communities they wish to reach, to trust in their ability to know their own needs. “If you were to go to any one of the regional house and ballroom alliances and be like, here’s this money, what would you do to get PrEP to be more utilized in your community…” Dr. Arayasirikul proposes, “you would see the solutions that I think our community so desperately needs.”
Wrap-around care
While stand-alone clinics can help to reduce perceived stigma for those who are concerned that bringing up PrEP could threaten their access to other important healthcare, like gender-affirming hormone therapy, proactive wrap-around care is also important. Dr. Arayasirikul highly recommends practitioners to move to an opt-out rather than an opt-in model. “In an opt-in model, the onus is on the patient to ask for PrEP,” they say. “I think routinely being in discussion about PrEP is important to help healthcare providers destigmatize and decolonize their own feelings about who should get PrEP.”
That conversation, Arayasirikul says, is also a great opportunity to learn more about your patient, even if they do choose to opt-out of PrEP. “A healthcare provider may learn… that [their patient] is concerned about PrEP’s efficacy, or potential contraindications. A conversation about PrEP may bring a healthcare provider deeper understanding into the other kinds of tools and prevention measures that a community is already employing.”
Diversity of tactics matters a lot when dealing with marginalized populations, whose decision-making around access to care is complicated by a number of intersecting vulnerabilities, Arayasirikul says. “In a world where there are many touch points to public health and to medical care, thinking critically about how we can integrate PrEP into those various touch points is important.”
Community, Culture, and Care
To address these many intersecting vulnerabilities, organizations like The Normal Anomaly are integrating the power of community organizing and engagement into their service offerings. They partner with community members to build and implement services, including working with both local drag performers and recognizable faces from programs like RuPaul’s Drag Race.
When The Normal Anomaly Initiative launched PrEPHer, they didn’t need to fight the uphill battle of getting their targeted communities to trust their offerings, because they were already established as trusted community members. “We’ve had years of building that relationship with community already…when we announced, our community was really excited because it was like, ‘okay, the organization that I know and trust is now doing work specifically centered for me.’”
When seeking buy-in from marginalized communities, the way to reach individuals is through those communities where trust already exists. Trust creates buy-in, buy-in creates engagement, and engagement creates impact. “When we engage community, not just as participants but when we engage community as consultants, people to help kind of build the programming,” Espeut tells me, “we’ve seen not just more excitement from students or from participants…but we’ve seen it be more impactful.”
As Dr. Arayasirikul points out, PrEP does not need to be prescribed by a doctor. It can be accessed via physician assistants, nurse practitioners, and in some states even pharmacists. “I think about how we can diversify the various kinds of prescribers for PrEP and offer PrEP in different ways.” Complex challenges like the intersecting vulnerabilities faced by Black trans women in the field of HIV prevention require creative and community-based solutions.
If you aren’t sure how to reach a community who you want to better serve, you should reach out to members of that community and trusted organizations already serving them. There is no lack of help available to providers who want to serve vulnerable populations better, if you are willing to seek out that help and ask for it.

Image by Polina Tankilevitch via Pexels
Power from Below, Strength from Within
PrEP works—but only when it is embedded in systems that recognize and address the intersectional vulnerabilities faced by Black trans women and other trans women of color. Biomedical tools alone cannot undo the structural harm caused by racism, transmisogyny, incarceration, housing instability, and healthcare discrimination. Real prevention requires more than a prescription; it requires a transformation.
That transformation must come through the alignment of policy, practice, and community leadership. It must center the voices and strategies of those most impacted, and it must work outside of the fickle systems which give and take funding and support on the whims of politicians. “The work that we are doing is necessary and is needed regardless of whether we have that funding right now,” Espeut tells me when I ask about how The Normal Anomaly Initiative is thinking about funding cuts in today’s political climate.
While national politics and federal funding remain unpredictable, especially for trans racialized healthcare, the solutions are already here, rooted in community. “The answer will not be a fix on a national or federal level…The answer is rooted within us, within community, within community-led organizations,” Espeut says.
Today, as access to preventive care like PrEP hangs in the balance of legislative rollbacks and judicial decisions, experts and community advocates are clear-eyed: the future of HIV prevention for Black trans women won’t be built from above, but from within. It will come from drag stages, digital clinics, house-ballroom alliances, and peer networks—where trust, care, and cultural fluency already live.
Equity is not theoretical. It’s practiced every day by those fighting to protect their own. The task now is to ensure they’re not doing it alone.
Appreciate my reporting?
Well Beings News can only exist with the support of our paid subscribers. Consider subscribing and upgrading to paid to ensure you get access to all our future reporting.
